Nina Paterson reports on a consensus-to-action project to develop best practice for respiratory disease in young people with cerebral palsy.

What happens when you take an Australian-led research consensus statement published at the height of the pandemic, focused on the prevention and management of respiratory disease in young people with cerebral palsy, and combine it with the passion and enthusiasm of members of one of the UK’s physiotherapy professional networks the Association of Paediatric Chartered Physiotherapists (APCP)?
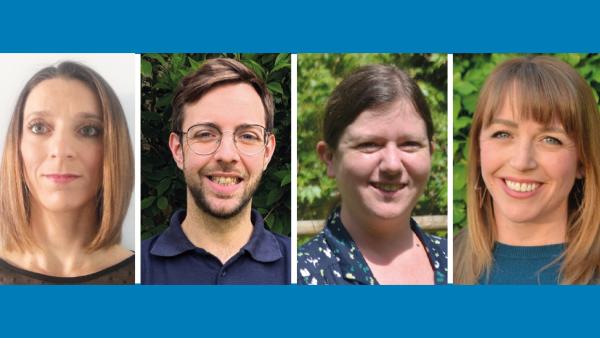
I spoke to Naomi Winfield, a lecturer at University College London and an independent children’s respiratory physiotherapist; Laura Lowndes, a clinical specialist paediatric respiratory physiotherapist at Cambridge University Hospital NHS Trust; Madeline Pilbury, a children’s physiotherapist from Stockport NHS Trust; and Jason Kettle, a trainee advanced clinical practitioner from Lincolnshire Community Health Services NHS Trust, to find out.
Let’s start at the beginning – Madeline and Naomi share their excitement about the original consensus statement – bringing together over 200 researchers and clinicians to develop consensus on best practice for preventing and managing respiratory disease in young people with cerebral palsy. Their excitement is justified, as Naomi notes ‘this is a patient group often neglected in the literature’.
Determined that interest in the new consensus statement didn’t fade, their own project consensus-to-action was born.
It’s aim? To bring that research to life by developing guidance and support to better identify and treat those at most risk.
And if those services don’t exist? Then as Madeline notes – ‘to get healthcare planners, commissioners, the government interested in this patient group, and support those in respiratory care to demonstrate need, identifying gaps between what they need and what they currently can provide is essential’.
And that’s where their new resources come in. The guidance supports new and existing children’s community respiratory services to develop and evaluate their impact. Alongside this, the team has also developed a respiratory risk matrix that can be used by multidisciplinary teams (MDT) to identify those most at risk, and who’ll need those services.
The team are rightly proud of the resources and the impact that two of the new services are already having [see case studies]. Naomi notes that it’s possible to make a big impact even with ‘a small team with a lot of passion’. She continues ‘if anyone else wants to do something similar, we are happy to share our experiences.’ So, if you are looking for ways to bring research to life, take them up on their offer! You’ll find the team at the Physiotherapy UK conference this year but see BOX for tips to get you started.
Rapid response respiratory service, Cambridge and Peterborough ICB area
The service has been running as a pilot since June 2023. Laura shares that while they are linked to an acute hospital, the team see themselves as community physios. Laura notes their motto ‘We’re where the patient is, not where staff are’, reflects that.
The service has three aims:
- Empowering patients and families to self-manage their conditions, offering training on things such as suctioning. They also offer support on how to spot the signs of respiratory problems so patients can get help as early as possible.
- Supporting other staff, offering training, joint treatment sessions and empowering the MDTs.
- Providing a rapid response service so that parents/carers can speak to someone within 24 hours.
There’s clearly a demand – the service has reached its 70th child. Early data is showing that the service is saving on avoidable admissions and bed days (around 60 per cent). These performance indicators alone have warranted an extra six-months of funding, and now the team are in the process of gathering qualitative data to strengthen their case.
Initial feedback shows meaningful impact – of children able to spend Christmas at home, children having a better quality of life and able to access schooling, of whole families less disrupted, members of the MDT – community nurses and palliative consultants – feeling supported and themselves also witnessing families now able manage their child’s complex needs at home.
Which leads us back to the consensus-to-action project. Laura hopes the risk matrix will empower others to identify those that need support, adding to the growing evidence that’s needed to ensure that services like hers continue and new services developed.
Small team, big impact
Thinking about doing something similar? Three tips from the team on getting started
Understand the landscape
The team needed to find out what community respiratory services existed in the UK, so they began with a scoping questionnaire.
Collaborate
The value of having an MDT focus is key. It’s clear that this underpinned the team’s approach from the project’s inception – publishing an article in the British Academy of Childhood Disability (BACD) newsletter to reach medics and healthcare professionals across the MDT, which led to APCP hosting a free webinar on behalf of BACD, with the lead author of the original research paper presenting and around a hundred people attending.
They hosted a Twitter/X-chat and connected with other physiotherapists including Rachel Knight Lorenzo [see Useful links] working on similar projects, and again looking beyond to the MDT, teamed up with speech and language therapists through the Paediatric Dysphagia Clinical Excellence Network.
Don’t be shy
The team looked for conferences to get their message out... King’s John Price paediatric respiratory conference, The Royal College of Paediatrics and Child Health, BACD… wherever they could promote their aims of sharing research, innovative practice and collaborating on projects to improve the respiratory health of children and young people with neurodisability, the team were there.
Complex needs rapid response respiratory service, Lincolnshire Community Health Services NHS Trust
Jason’s team also supports individuals with complex needs. The service started as a pilot in 2019 with 125 patients seeing 80 per cent reduction in hospital admissions. Since then, the service has expanded, first to include adults with complex needs up to aged 25, and last year it became an all age service, something Jason sees as absolutely critical as those with complex needs are now living longer but specialist support into adulthood is sparse.
Like Laura, Jason believes having a tool such as the risk matrix that other therapists can use to identify patients who need services like his, will be beneficial. He agrees that ‘by identifying those who need these type of services, we’ll be able to identify gaps in service and better make the case for them to be commissioned’.
Meet the team
Want to find out more? Catch the team at the CSP annual conference or join their webinar on 17 September.
Find Out More
Number of subscribers: 1