Each month, the CSP’s professional advisers share advice and guidance on a topical matter
Knowing our population is the first step towards being able to improve health inequity, which can in turn reduce health inequality optimising patients’ chances to achieve their best health outcomes.
As physiotherapists, we are in an excellent position to understand the unique health needs and the multi-factorial barriers to engagement of the populations which access, or struggle to access, our services.
Stark examples of health inequality are evident across the UK. For example, Glasgow life expectancy in men goes down by two years for every station on the trainline travelling from Jordanhill (78 years) to Bridgeton (63.7 years).
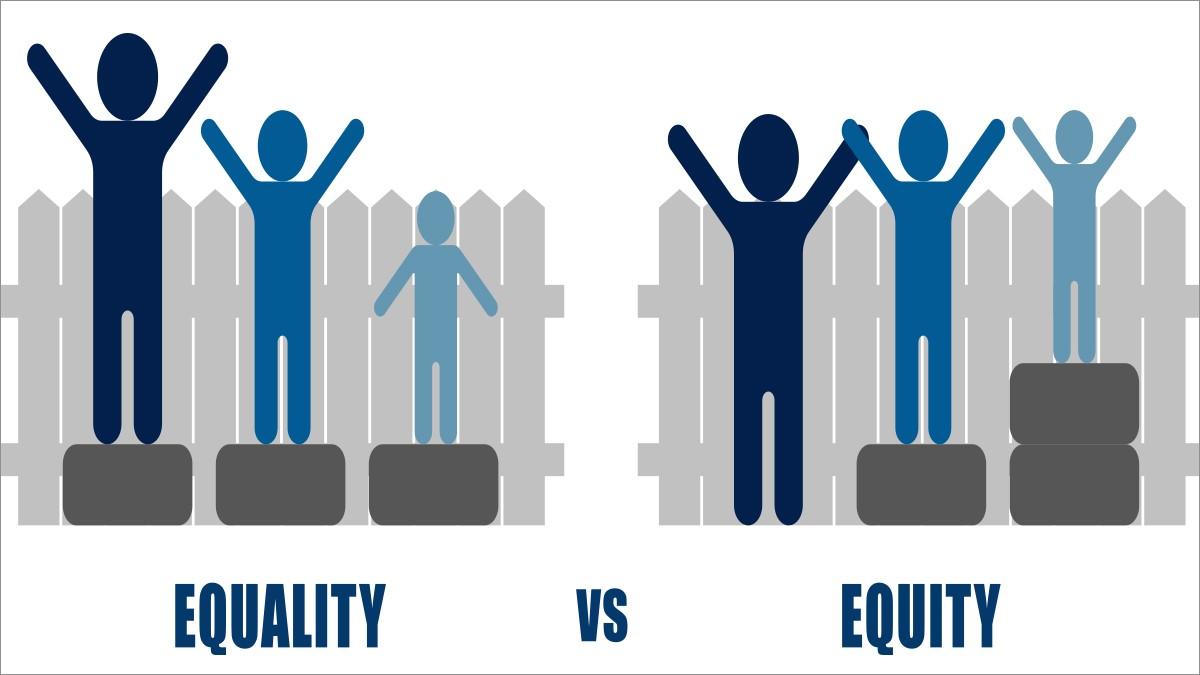
Health equality and health equity are not the same thing
Equality is giving people the same opportunities without making adjustments to meet individuals needs.
Equity is taking steps to enable people, by providing what they need, to reach their best health outcome over and above equality of access.
What can we do to understand our population?
The NHS Long Term Plan (2019) outlined the need for more action on prevention and health inequalities and with the King’s Fund’s AHP framework for tackling health inequalities we now have strong practical guidance of how to contribute to this change.
The Framework encourages all AHPs throughout their career to contribute towards improving health inequalities via three approaches: raising awareness, taking action and optimising advocacy through six routes to change:
1 Self: everyone’s individual contribution counts – such as increasing your own awareness of health inequalities and considering what unconscious bias you have which could impact your practice. There are excellent resources available such as the King’s Fund’s Health Inequalities in a Nutshell paper.
2 Patients: is your patient at risk of experiencing barriers to healthcare such as learning difficulties, poverty and deprivation or low health literacy? What can you do to improve their equity of access? Could these steps benefit other patients?
3 Clinical teams, pathway and service groups: does your service collect and effectively utilise demographic data about patients?
Are there any gaps in the information you collect? Does the data tell a story about an underserved community in your patient population?
Practical example: You want to make your MSK clinic hours more accessible. You survey existing patients about convenient clinic opening hours–the outcome is that the existing hours are fine.
Consider: With this approach you are not reaching those who struggle to access the clinic.
Look for ways to include opinions from a much wider population that may be struggling to access the service - such as asking via local GP practices or local orthopaedic teams.
4 Communities and networks: Working together across services is essential to ensure the needs of your population are fully understood.
Consider how health inequality may impact at different junctures in patient’s health journey. Is there anything you could do to advocate for patients as they transition from your service into another service? Do groups of patients get lost along the way?
Are the referrals/ self-referrals received by your team reflective of the population in that local area – if not, why not? Can awareness be more widely raised in different ways and to different audiences (for example faith groups, online social groups, local cafes and libraries).
5 Systems: If there are known populations not accessing certain services it is the duty of the system to reach out to where those communities gather.
However, everyone can be proactive in building relationships within the system to promote engagement - for example building relationships with relevant community groups.
6 Nurturing the future: How can we plan for the changing needs of our population? Population health changes do not provide swift outcomes. NHS England suggests that population health changes may be felt 15-20 years down the line but the decisions we make today are crucial for the healthy lives of the future population.
Take a leaf out of the Future Generations Act in Wales, which requires public bodies to think about the impacts of its decisions to build cultural change in the long-term. Consider how changes made to services today (such as closure of treatment spaces) may have an impact on the health of your population in years to come.
Links and resources
- My role in tackling health inequalities: a framework for allied health professionals (June 2021)
- NHS Long Term Plan (2019)
- Health Inequalities in a Nutshell (August 2021)
- Future Generations Wales
Reflective activity
- Reflect on a patient who is not improving.
- Are avoidable health inequities limiting your patient’s outcome? What might you consider?
- What is the patient’s level of health literacy?
- What is their level of knowledge retention?
- Could there be cultural or linguistic barriers?
- Are there socio-economic barriers?
What steps can be taken to reduce the impact of these barriers?
Select an approach from the King’s Fund framework (awareness, action or advocacy) and reflect on what steps you can take to improve health equity in your service to improve your patient’s engagement and outcome.
The CSP's Professional Advice Service
This service gives advice and support to members on complex and specialist enquiries about physiotherapy practice, including professional practice issues, standards, values and behaviours, international working, service design and commissioning, and policy in practice. Find out more from out Professional advice team here.
- Clare Aldridge and Hannah Morley are CSP professional advisers
Number of subscribers: 1
