Lymphoedema is a progressive, long-term condition where early intervention from physio staff and others is vital, as Jane Rankin explains.
Lymphoedema arises when the lymphatic system inadequately fulfils its function of regulating fluid balance in tissue spaces. It is a long-term condition with physical, emotional, financial, and social side-effects.
LNNI’s key messages
- Wear your garment every day
- Take good care of your skin
- Be active!
- Think about your weight
Lymphoedema Awareness Week runs from 5 - 11 March: see further details.
Primary lymphoedema can develop as a result of a genetic fault in the lymphatic system appearing at or around birth, or later in life. Secondary lymphoedema can develop as a consequence of trauma or from conditions such as cancer, obesity, infection, immobility and venous disease. Lymphoedema is progressive; if untreated, permanent tissues changes will occur. The outcomes are better, and the condition managed more effectively and efficiently, if diagnosed early.
Other chronic oedemas, and lipoedema, are now being referred into lymphoedema services, impacting on commissioned resources and waiting lists. The National Lymphoedema Partnership (NLP) produced a 2015 definition of chronic oedema to support this change:
Chronic oedema is a term used to describe a group of conditions characterised by the presence of swelling within tissues of the body, caused by the accumulation of excess fluid within the interstitial space of the affected area.
Oedema most commonly affects the lower or upper limbs, but may also affect midline structures such as the head and neck, trunk, breasts or genitalia.
Qualifying term
The term ‘chronic oedema’ is often used interchangeably with ‘lymphoedema’. Oedema results from an imbalance between capillary filtration into and lymphatic drainage from the interstitial space. Although the term ‘lymphoedema’ suggests that the oedema is caused by a lymphatic abnormality, in every case of chronic oedema there will be some impairment of lymphatic drainage, either through an underlying abnormality (‘primary’ or ‘secondary’) or through ‘lymphatic failure’ as a result of the capacity of the lymphatics being overloaded.
The degree to which the lymphatics are, or become, affected may influence the clinical presentation of the oedema, the subcutaneous tissues and skin. Where there is an impairment of lymphatic drainage, over time, the fluid component of oedema may become replaced by fibrosis and/or adipose tissue. (Full definition and qualifying terms available at www.thebls.com.)
Partnerships with local bariatric services are useful; likewise the impact of exercise is essential, with water-based activity proving to be very successful for lymphoedema and lipoedema.
Complex decongestive therapy (CDT) describes specialist lymphoedema management. This must be a partnership of therapist-led activity, lifelong self-management and GP follow up (Macmillan 2011).
CDT is the first stage of management: compression via multi-layer bandaging/compression garments, manual lymphatic drainage, skin care and exercise.
Other adjuncts including Kinesiotaping and electrical modalities are also available.
The British Lymphology Society (BLS) created a bariatric lymphoedema pathway to support this challenge. Self-management is essential for success including adherence to wearing compression, increasing levels of activity/weight management and good skin care. This will improve quality of life for those affected, and reduce NHS costs.
In addition the International Lymphoedema Framework (ILF 2012) supports specific lymphoedema liposuction when oedema has been replaced by adipose tissue. Other techniques, including node transplant and vessel anastomosis, are evolving. See also ILF practice guidelines (2006).
- the CSP publication Physiotherapy Works: Lymphoedema features an award-winning service that estimates that every £1 spent on lymphoedema services saves the NHS £100 in reduced hospital admissions
- cellulitis often leads to hospital admissions. See BLS guidelines (PDF)
- lymphoedema teams, including physio staff, should have education roles as part of their remits, and those working with ‘at risk’ groups should receive awareness education to improve diagnostic skills and referral pathway awareness. fl
Jane Rankin is a physiotherapist and lead for the Lymphoedema Network Northern Ireland (LNNI)
Prevalence
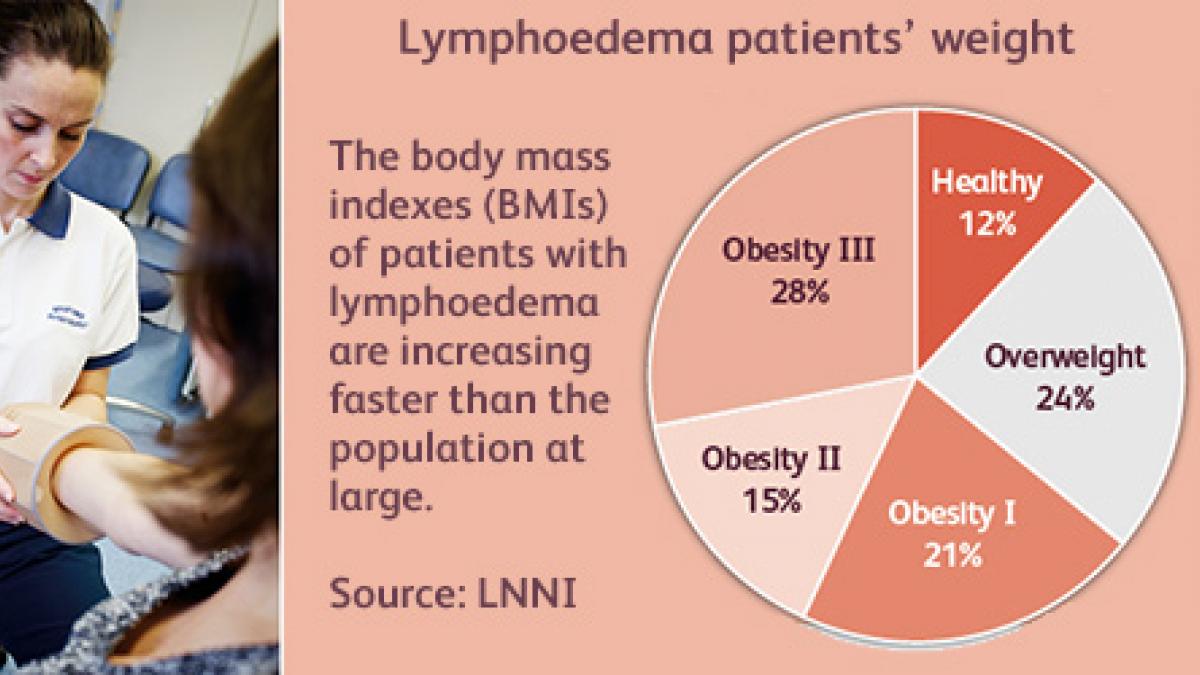
Regional registers suggest that currently published figures underestimate the prevalence of lymphoedema in the UK. The regional figures highlight the increasing impact of an ageing population, obesity and improved cancer survivorship.
| UK region | Prevalence rates |
|---|---|
| Wales | 5.49 per 1,000 (Thomas 2017) |
| Northern Ireland | 4.85 per 1,000 (Rankin 2017) |
| Scotland | 7,000 to 21,000 of the population (SMASAC 2013) |
| England | 3.99 per 1,000 (* Moffatt 2012) |
More information
- British Lymphology Society
- Lymphoedema Support Network
- This article is fully supported by Dr Jackie Gracey, chairperson, the Association of Chartered Physiotherapists in Oncology and Palliative Care
References
- CSP (2012) Physiotherapy Works: Lymphoedema
- International Lymphoedema Framework (2012) Surgical Intervention – a position document on surgery for lymphoedema, and (2006)
- Best practice for the management of lymphoedema,LNNI key messages (2015)
- Macmillan (2011) Lymphoedema Specialist Services: an evidence review
- Moffatt C, Pinnington L (2012) Facilitating Development of Community Based Lymphoedema Services through Clinical Education. Project Evaluation Report, University of Nottingham/Derby Hospitals NHS Trust Rankin, J (2017)
- LNNI, via email
- SMASAC Short Life Working Group on Lymphoedema (2013)
- Thomas M (2017) Welsh Lymphoedema Network, via email
- Thomas M (2017) Welsh Lymphoedema Network, via email
Author
Jane Rankin is a physiotherapist and lead for the Lymphoedema Network Northern Ireland (LNNI)Number of subscribers: 3
