Clinical guidelines on assessing and treating patients with metastatic spinal cord compression (MSCC) have been developed for physiotherapists and occupational therapists (OTs).
The lead authors (OT Nicola Evans and clinical specialist physio Paula Finlay) used research evidence, expert opinion and professional consensus to produce guidance for colleagues in the acute sector in Northern Ireland.
What happens in MSCC?
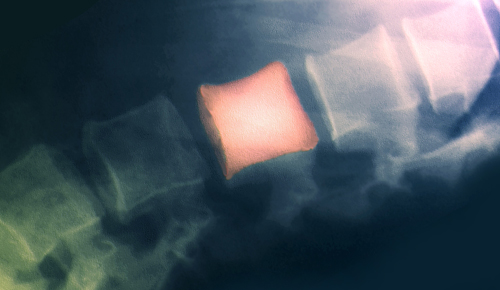
There is compression of the spinal cord or cauda equina by direct pressure and/or induction of vertebral collapse and instability, by metastatic spread or a direct extension of malignancy that threatens or causes neurological disability.
Who gets MSCC?
A major cause of morbidity, MSCC occurs in from five to 10 per cent of all patients with cancer. The incidence is expected to rise as more people survive cancer.
In about 85 per cent of cases, MSCC results as a consequence of metastases from a primary tumour. Cancers of the lung, prostate and breast are at the most likely to cause MSCC, accounting for 50 per cent of cases. Other cancers frequently associated with MSCC include lymphoma, renal cancer, multiple myeloma, melanoma and sarcoma. However in from 10 to 20 per cent of cases, patients with MSCC will have no prior malignant diagnosis and MSCC will be the first manifestation of cancer.
When to seek help for suspected MSCC
MSCC is an oncological emergency requiring urgent investigation and immediate treatment. Red flags for MSCC are the presence of one or more of the four cardinal signs and symptoms of MSCC and a history of cancer. High risk conditions include lung, breast and prostate cancer or bone metastases. Early reporting, detection and treatment are vital.
Diagnosis is based on MRI findings. National Institute for Health and Care Excellence (NICE) MSCC guidelines (2008) state that an MRI should be done within one week for patients with spinal pain suggestive of spinal metastases. For patients with spinal pain and neurological symptoms suggestive of MSCC, MRIs should be done within 24 hours.
Definitive treatment, if appropriate, should commence before any further neurological deterioration and ideally within 24 hours of a confirmed diagnosis of MSCC. Medical management may involve radiotherapy, surgery, vertebroplasty, spinal bracing, pain control, steroids, anticoagulant therapy and bisphosphonates.
Referral and assessment:
The guidelines say that suspected and confirmed MSCC patients should be referred for physio and OT on admission. Physio and OT assessments should be carried out within 24 to 48 hours after admission and should commence with a thorough examination of the patient’s history.
There should be a detailed examination of the four cardinal signs and symptoms of MSCC. Pain, sensation, proprioception, muscle power and tone, clinical observations, respiratory function, range of movement, balance, posture and alignment should be assessed. An assessment should also be made of functional mobility, fatigue and exercise tolerance, seating/wheelchair needs, skin integrity, swelling, deep vein thrombosis presence/risk, lymphoedema, bladder and bowel function, social and occupational needs, psychological wellbeing, cognitive processing and signs of autonomic dysreflexia.
Supportive care and rehabilitation
Care of the threatened spine:
- patients with severe mechanical pain suggestive of spinal instability or any relevant neurological signs or symptoms should be treated as having
- unstable MSCC until MRI results and the medical team confirm a diagnosis.
- the stability of the spine and the level of mobility allowed should be agreed by medical staff and the multidisciplinary team before starting active rehabilitation.
- clinical vigilance should be exercised throughout rehabilitation with regular assessment and documentation of pain and neurology in the patient’s notes.
Care and rehab in ‘unstable MSCC’
The guidelines cover positioning in bed, safe moving and handling, use of collars/bracing. They look at bed exercises, respiratory care, preventing contractures and spasticity control.
Care and rehab in ‘stable MSCC’
Patients need graduated mobilisation with strict pain and neurological monitoring.. Other topics include progressive exercise and rehab, education and discharge planning. fl See also page 26
References
- Metastatic spinal cord compression: Diagnosis and management of adults at risk of and with MSCC (NICE 2008).
- To see the full version of the guidelines summarised here (and an extensive review of the literature in evidence- based tables).
Four cardinal signs and symptoms of MSCC
- pain: local neck or back pain or radicular pain, radiating to the limbs (arms or legs), or as a tight band around the chest or abdomen.
- depending on the level of compression. Pain is mechanical in nature and often the first symptom.
- motor dysfunction: characterised by weakness or paralysis, ataxia, unsteadiness, difficulty walking and legs giving way.
- sensory dysfunction: may cause anaesthesia, paraesthesia, hypersensitivity and proprioceptive loss bladder and bowel dysfunction: urinary retention, constipation and incontinence.
MSCC priorities
- better patient and staff education and earlier reporting of MSCC signs and symptoms.
- earlier detection and diagnosis of MSCC with timely access to MRI scanning (within 24 hours if MSCC is suspected)
- prompt treatment and timely access to orthopaedic advice and intervention if required.
- improved reporting and prompt documentation of spinal stability status and mobility allowed.
- improved clinical vigilance with close monitoring of pain, power, sensation and bladder and bowel function (see four cardinal signs box, below left).
- early referral to physios and OTs and early discharge planning from admission onwards for patients with MSCC in the acute sector.
- adequate and timely provision of supportive care, rehabilitation and equipment and adaptations in the acute and community sectors.
Managing MSCC
The guidelines provide specific recommendations on the following topics:
- referral.
- assessment.
- supportive care and rehabilitation for those with unstable MSCC.
- supportive care and rehabilitation for those with stable MSCC.
- end of life considerations.
Author
FrontlineNumber of subscribers: 0
